Improving Communication With Families in the Intensive Care Unit.
Communicating uncertainty in the intensive care unit (ICU) to patients and families is challenging given multiple factors, including lack/limited data, complication, and time pressure to manage sick and unstable patients [1]. This project aims to improve communication of uncertainty with patients and families in the ICU to enhance the quality of care and patient prophylactic past being honest and transparent and disclosing information in a timely manner to build upwardly trust with the healthcare team.
The project volition utilize computer science to facilitate communication and share data. Leadership is a primal in "times of uncertainty." This project volition add value to patients' advancement and trust buildup with the healthcare team by ensuring proper advice from the healthcare squad to come across the expectations and needs of families and patients [2].
Major and pocket-size focuses
The major focus is to amend the quality of intendance by improving communication during uncertain times, as divers by the first 24 hours of ICU admission.
Small-scale focus is to utilise informatics to heighten communication and improve patient prophylactic by enhancing better and timely communication with the family unit.
Problem statement
In that location are uncertainties surrounding diagnosis, handling, and prognosis in ICU. Patients and families ordinarily look for more than information to keep them informed, bring disclosure, and reflect the high care quality they received [two]. Oftentimes, communicating prognostic uncertainty in ICU tin can be misleading or confusing to patients and their family unit members [ii]. In an interview conducted with 90 family members of patients who died regarding "communicating prognostic incertitude," less than one-half of the family members were non satisfied with communicating the patient'southward likely upshot [2].
The project'due south scope will be patients admitted to ICU in the commencement 24 hours to improve the communication of uncertainty between the ICU team and patients and family members, assess response, develop an action plan, and provide support. Follow up and update when clinical condition changes or new data is bachelor. The project will not address incertitude measurement, adventure assessment, and evaluating how physicians respond and deal with doubt.
Furthermore, effective communication has been shown to improve satisfaction and finish-of-life care experience and is associated with loftier-quality care from patient and family perspectives [ii]. The project will aid meliorate the quality of care delivered in ICU to patients and their families by improving communication and support through decision-making under uncertainty and edifice trust.
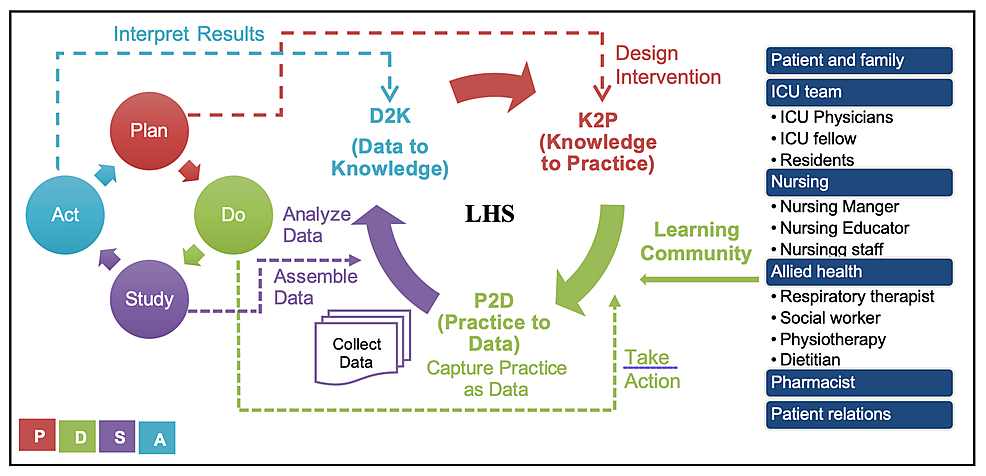
Learning customs
The stakeholders are patient and family unit members, ICU team, nursing manager, nursing educator, nursing staff, centrolineal health, social worker, and pharmacist.
Sponsor: Chief of ICU.
Team leader: Physician atomic number 82.
Projection team: ICU md, nursing manager, and social worker.
Aim statement
To amend communication of uncertainty in ICU with patients and families in the beginning 24 hours of admission past 75% within ane yr using quality metrics indicators.
SMART Aim
Specific: Focusing on improving advice uncertainty in the ICU with patients and families in the first 24 hours of ICU access. The focus is "family-centered intendance" to improve the quality and feel of families in ICU past providing back up [3].
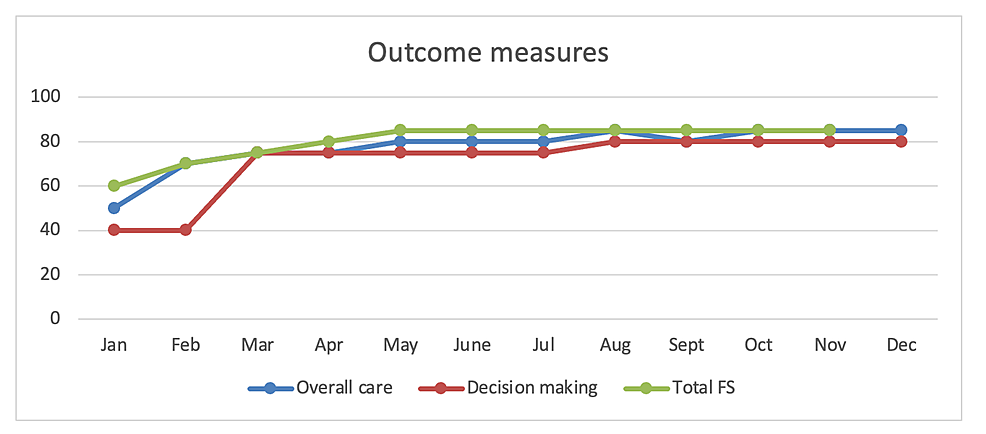
Measurable: By measuring timely communication and satisfaction of the patient and family experience using the Family unit Satisfaction with Care in the Intensive Care Unit (FS-ICU 24) questionnaire, which has been validated, and 1 of its components is communication with the ICU team [4,v]. The questionnaire correlates with the quality of care [iv]. FS-ICU 24 is self-administered and takes 10-15 minutes to complete [4]. The aim is to achieve at least a score of 75 or more than, which correlates with very skilful [iv]. Past collecting feedback from physicians and nurses, we go insight into what works and the challenges of communicating uncertainty.
Attainable: Communication with family is part of daily encounters in ICU with the ICU multidisciplinary team. Nearly of the advice happens by physicians and bedside nurses. A total of 87% of surrogate decision-makers in semi-structured interviews of 179 surrogates to patients in ICU with a high risk of bloodshed wanted prognostic doubtfulness to be discussed by physicians, acknowledging "doubt is inevitable" [half dozen]. Finding, along with the study by Krawczyk and Gallagher (2016), shows that families and surrogate determination-makers capeesh open and honest advice [six].
Relevant: Communication with family is function of the A-F ICU liberation bundle ("A: Appraise, prevent, and manage pain; B: Both spontaneous awakening trials and spontaneous breathing trials; C: Option of analgesia and sedation; D: Delirium: assess, prevent, and manage; E: Early mobility and exercise; F: Family engagement and empowerment"), which is recommended past the Society of Critical Care Medicine and used by ICU teams daily during rounds [7]. The bundle has been shown to improve outcomes in ICU, and the F component refers to family engagement and empowerment [8]. It is also an essential part of "shared conclusion-making" in the ICU to constitute patients' values and care goals [eight,9]. Information technology aligns with the concept of "family unit-centered care," which is defined as "an approach to health care that is respectful of and responsive to individual families' needs and values" [3]. As from surrogate decision-makers and families, the relevance of discussing dubiety from their perspective is to let them to be prepared mentally for the worse outcome, hope for the best, brand decisions, and promote trust with the ICU team [6].
Time-jump: The projection volition run for 12 months, with a monthly review of both the FS-ICU24 questionnaire and feedback from the staff to arrange or make a change.
Proposed intervention
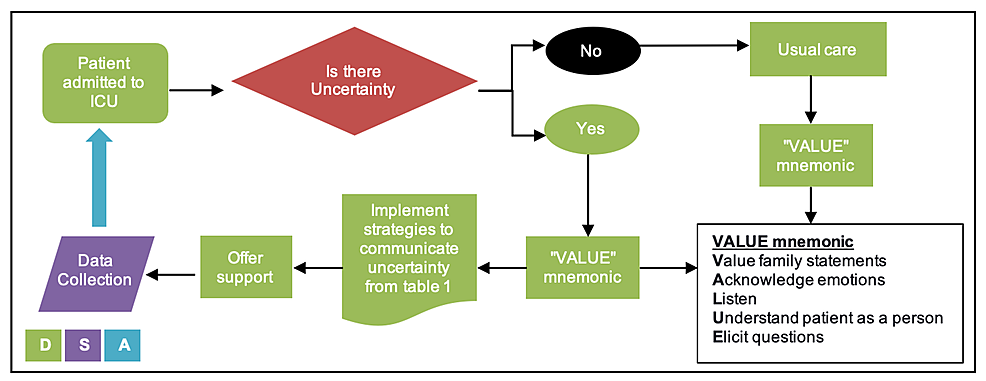
Following the learning wellness system in data to knowledge (D2K) stage (Figure ane), identify a need to improve communication with family members of critically ill patients in the ICU, peculiarly in the coronavirus disease 2019 (COVID-xix) pandemic, where challenges include remote communication, more uncertainties resulting in anxiety and fright. Our focus is mainly on quality improvement using PDSA (Program, Do, Study, and Deed) bike for rapid testing and implementing changes. The project starts past planning a workflow (Effigy ii) and advice tools to be used by the ICU team that follows a structured approach of communicating uncertainty from evidence-based recommendations (Table 1) [x]. The mnemonic VALUE (Value family statements, Admit emotions, Heed, Understand the patient as a person, Elicit questions) volition be the usual intendance of communication [3].
The time of assistants volition be with the first encounter and on every subsequent meeting with family members. These time points tin can exist during a scheduled family unit coming together or when given an update. Family members are offered back up during the process. The back up can be provided by the ICU team, nursing staff, social workers, and spiritual care. The response and feedback from patients, family unit members, and providers will be collected. Studying monthly reviews of responses and feedback to place any changes to the process or modifications to the workflow.
Past structuring bear witness-based communication tools and workflow to back up family members during their ICU experience, we tin can improve communicating doubtfulness to family members of critically sick patients in ICU and identify and provide back up to those who need it. The timeline of PDSA volition exist equally follows: iv months for a plan, 12 months for do, and monthly for study and human activity. The FS-ICU 24 tin be accessed online [five].
Measurement
The master outcome is patients and family satisfaction with ICU experience to accomplish a score of 75 or more, which correlates with very good [4]. Secondary outcomes will mensurate process and structure metrics, as shown in Table 2.
The data review will be done monthly by the project team to assess the ongoing need for adjustment and comeback (Figure 3). The data review ties to the written report and activeness phases of the PDSA cycle. A baseline data collection will be done during the planning phase for comparing.
Challenges
We need to anticipate multiple challenges and barriers; the most important i is related to the COVID-19 pandemic and the limitation of resources. Patients admitted to ICU with COVID-19 add another layer of complexity to the doubt and the fearfulness and anxiety associated with it. The following are the challenges and suggested strategies [13-15]:
i. Staff training: This will require staff training to deliver effective communication, documentation of encounters, and duration. It tin can be done through learning modules, printed cards, guideline documents, and structured notes.
two. COVID-19 pandemic: Since the COVID-19 pandemic started, a lot of innovations accept been tried and shared. Those innovations are mainly surrounding the delivery and the communication of care. Due to restrictions on hospital visits, virtual visits accept been offered as a manner of communication. Of form, the challenges are usually in familiarity with engineering, malfunction, lack of face-to-confront interaction, and loss in translation. This tin exist made improve by having infrastructure, a reliable and secure platform, and allocating designated person to communicate.
three. Time challenges: Due to the nature of ICU, fourth dimension can be challenging to meet family members, and commonly, meetings are scheduled. With the restricted visiting hours, families are non by the bedside as at times of pre-COVID-19 pandemic, and this puts some force per unit area on the ICU team to update families later their daily rounds. Suggest identifying team members responsible for communicating updates with family members to aid be consistent, build rapport, and accept off some of the team'due south pressure level.
four. Resources limitation: These include limited access to the social worker for every patient and family member. Propose identifying those who volition likely require referral back up.
5. Process: There are opportunities to improve communication in two situations:
(a) Transfer from ICU: Communicating with family members upon transferring patients out of ICU is important. Those ordinarily are emotional times for fright of returning to ICU, break-in intendance, and what is next [fourteen]. The assurance from the ICU team on communicating the transfer to family unit members should also include the follow-up past the rapid cess of disquisitional events (RACE) squad.
(b) Stop-of-life care/palliative care: These conversations require skillful communication to ensure discussions of goals of care are met and the family unit feels supported during the process.
6. Structure: This includes the following:
(a) Culture: In that location might be some reservations to admit uncertainty openly, and a culture of "incertitude is inevitable" is encouraged to help facilitate those types of discussions. Some patients and families from specific backgrounds do not similar to know. Thus, in the recommendations in Table 1, explicitly assessing the desire to know the data is the first pace to establishing their perspective.
(b) Incentive: Hospitals might want to improve communications with family unit members in the ICU by hiring more support personnel and investing in continuous improvement projects to improve the process.
(c) Champions: Along the style, it helps to identify champions from the ICU team and family members as advocates to support others.
seven. Acknowledgment and trust: Once the ICU squad and family acknowledge uncertainty, trust can be congenital toward a common goal that both are working toward achieving. Advice is a vital part of the trust framework that is suggested past van der Voort and Lemmers in a contempo review [15]. The downside of acknowledging dubiousness is defoliation past the family members. This can be avoided by explicitly mentioning the steps taken to investigate and manage and the timeline expected. Assigning one person to communicate with from the ICU team and a spokesperson from the family unit help avoid misinformation and mixed messages and lessen the defoliation.
Sustainability
The projection improves everyday communication with family members in the ICU to lessen the uncertainty and provide support. The project tin can be hands incorporated into the daily A-F ICU liberation bundle, the showtime come across with family, every encounter, and scheduled meetings.
Working with the information technology (It) department to design a form integrated into the electronic patient tape (EPR) tin help the ICU squad conduct and document the meeting. Integrating the project into residents' and fellows' teaching will expand and ensure sustainability through training and EPR documentation.
Given that communication is a crucial part of the trust framework, and perceived quality of care is linked to patient and family satisfaction, leadership from the infirmary and family members will ensure sustainability and provide the back up needed to maintain the construction. These include hiring boosted supporting personnel, incentive, and investing in a reliable and secure platform to behave the virtual meetings.
Proceed to measure FS-ICU 24, the bike fourth dimension to better early advice, and support needed. To convey the information, use the ICU board to brandish FS-ICU-24 results monthly.
Scalability
For scalability, looking at 5 elements:
1. Effectiveness: Given the importance of improving communication with patients and families, especially in critical care in times of uncertainty, the project tin can expand to other areas that bargain with incertitude, including the emergency department, chief care, internal medicine, and surgical departments. The concept of communicating uncertainty starts after establishing rapport with the family unit using either the VALUE mnemonics or other communication skills methods then using the proposed recommendations suggested by Simpkin and Armstrong (2019) [10].
2. Education and training are key to performing communication skills. This will require an added session to the ICU fellowship curriculum and to rotating ICU residents to hash out how to communicate doubt. Staff training and online module volition help with sustainability.
3. Resources: Need training and infrastructure to support boosted resources for family members, including support personnel, volunteers, and hiring an boosted social worker.
4. Cost: Might need to hire back up personnel trained to provide emotional support equally required.
five. System: The crucial office is the back up of families when dealing with incertitude and giving thoughtful consideration to putting a support organization in identify that they tin admission 24/7 and partner with the community for rapid access.
The programme for broadcasting volition involve writing upward our ICU experience for disquisitional care centers to implement. The topic could be discussed in a formal interdepartmental ground round with internal medicine and the emergency section on a hospital level.
It is crucial to communicate clearly with the patients and families during critical care admission [2]. The dubiousness surrounding the diagnosis and prognosis in the ICU causes many miscommunications and can pb to misleading information if not communicated correctly [2]. Therefore, information technology is important to establish a communication tool for these scenarios to avoid the consequences of miscommunications. While keeping an open channel is vital, having assigned members who communicate with family establishes rapport and trust-building [3]. This is done as part of the A-F bundle during daily ICU rounds likewise as whenever there is a change of status [7]. This encapsulates the patient and family-centered intendance model in ICU by improving the communication with its members [2,viii].
During the COVID-19 pandemic, the apply of engineering has increased to permit for social distance [xvi]. This has taken the form of using video calls with family, which has been incorporated in ICUs to enable families to attend rounds nigh and communicate with the ICU squad [17]. Offer alternative methods of communication will need to be reliable and secure. When possible, incorporating informatics to guide and document advice with families is an integral office of the patient medical record. This will besides help track the timing and frequency of advice.
The proposal will accept an impact on safety and quality by allowing for open and honest communication and keeping the patient at the center of care. This will also empower families and provide needed support to help with care during ICU admission and transition of care. As discussed above, challenges and limitations are of import to identify and address. The project will need a continuous iteration of the PDSA cycle to go along incorporating feedback.
The project presents a unique structured tool in communicating uncertainty during the ICU stay. This will positively impact safety and quality by engaging patients and families with the ICU team. Using a structured communication tool helps with conveying the information while allowing for dialogue and discussion. Future enquiry studies are needed to address the gap in communicating dubiousness in ICU.
Source: https://www.cureus.com/articles/77448-improve-communicating-uncertainty-in-intensive-care-unit-with-patient-and-family-icu-pf
0 Response to "Improving Communication With Families in the Intensive Care Unit."
Post a Comment